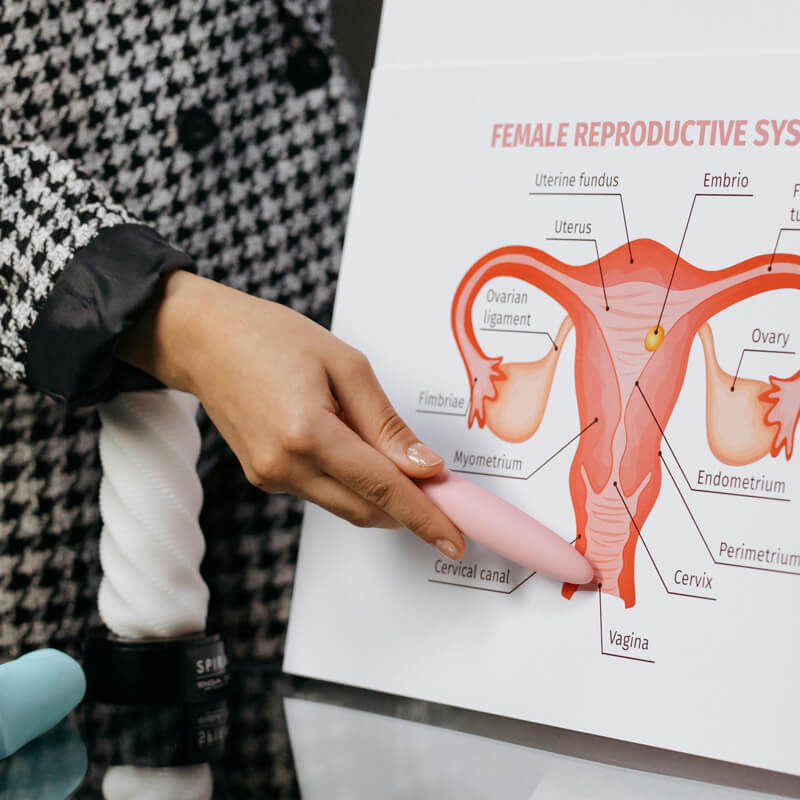
Women often face unique health challenges—especially when it comes to digestive and pelvic floor issues.
But let’s be honest: many of these topics are still considered “taboo,” which leads to confusion, delay, and unnecessary suffering. So let’s change that.
Here are 5 of the most common questions I get from female patients—answered directly, without fluff or embarrassment.
1. Is it normal to have pain during bowel movements, especially around my period?
Short answer: Not necessarily.
Mild changes in bowel habits during your period can be normal, but pain—especially sharp, burning, or cramping pain—is not something you should ignore. It could be caused by hemorrhoids, anal fissures, or even endometriosis infiltrating the bowel. If it’s cyclical and linked to your period, it’s worth investigating further.
2. Why do I have a constant feeling of pressure “down there”?
That heavy, dragging feeling in the pelvis or rectum might be more than just stress or fatigue. It can be a sign of pelvic floor dysfunction, rectocele, or even prolapse. These conditions are surprisingly common in women who’ve had children, especially vaginal births. The good news? There are effective treatments—from physiotherapy to surgery, depending on the severity.
3. I’ve had hemorrhoids for years—do I really need surgery?
Not always. Chronic hemorrhoids can often be managed conservatively with diet, medication, lifestyle changes, or ambulatory procedures ( e.g. rubber band ligation or sclerotherapy). But if they’re causing bleeding, prolapse, or interfering with your daily life, it may be time to consider a surgical or minimally invasive solution. The key is individual assessment—there’s no one-size-fits-all approach.

4. Can stress or anxiety really mess with my digestion?
Absolutely. The brain-gut connection is very real, and women are particularly prone to stress-related digestive issues like IBS (Irritable Bowel Syndrome). Bloating, cramps, constipation, or sudden urgency can all be linked to emotional and psychological stress. In some cases, working with a psychologist, stress management techniques, or even cognitive behavioural therapy (CBT) can be just as important as medical treatment.
5. I’m embarrassed to talk about this… but I sometimes leak gas or stool. What can I do?
First of all: you’re not alone, and you shouldn’t be ashamed. Anal incontinence or loss of control over gas or stool can happen after childbirth, surgery, or even due to nerve or muscle weakness. It can often be improved with pelvic floor rehab, dietary changes, and sometimes surgical correction. But it won’t improve if you keep it a secret. Speak up—we’ll figure it out together.

Final Thoughts
Women’s digestive and pelvic health is often overlooked or dismissed. But you deserve answers—and solutions. If you’re dealing with any of these issues (or something else entirely), don’t wait. The sooner we talk about it, the sooner you can start feeling better.